C4 Stroke Ward's Journey to Bronze Accreditation
Ward C4 Stroke is making significant strides toward earning the Bronze Award through the Ward Accreditation and Improvement Programme—a key initiative within the Health Board aimed at embedding excellence, eradicating avoidable harm and cultivating a supportive and high-performing culture within our teams.
The Ward Accreditation and Improvement Programme is designed to recognise teams that achieve outstanding results and outcomes for patients while fostering a continuous improvement mindset. For staff, it provides a shared understanding of quality and a clear framework for prioritising and tracking improvements that can be visualised on a dashboard, accessible to all staff. Accreditation is not only about improving patient outcomes but also about valuing staff contributions, enhancing job satisfaction, and promoting a culture where everyone's voice matters.
We caught up with Sarah Ferguson, C4 Stroke Ward Manager, and Vicki Burrell from the Shaping Change team to find out more. Sarah reflects on the initial challenges: ‘Being nominated for accreditation was daunting at first, and I experienced a lot of imposter syndrome. But I realised it was something to be proud of, not just for myself, but for the whole team.’
‘The Ward Accreditation (WAI) team spent time on the ward speaking to patients and staff, observing care delivery and patient records in order to get a true reflection of life on the ward. I wanted to get an honest audit, so I made sure not to tell anyone the visits and audits were happening. The WAI team also looked at other digital information, such as Datix records, Health Roster, SafeCare, and Patient Experience reports. A staff survey was also conducted with the support of the Patient Experience team to inform the overall feedback they gave us and we were able to see this visually on a dashboard.’
‘Although we did quite well, hearing the feedback was challenging. However, I was determined to make a success of the improvements and focus in on what we could do’
The team decided to focus on one critical area—monitoring lying and standing blood pressure, a vital safety measure for stroke patients. This focus was inspired by past incidents where gaps in compliance led to unsafe situations. By involving the team in the decision, Sarah fostered a sense of ownership, demonstrating that everyone plays a role in delivering safer patient care.
‘Lying and standing blood pressure (also known as postural hypotension) is the measurement of blood pressure when transitioning from lying down to standing up. It is hugely significant for stroke patients as we often administer many antihypertensives in the acute phase of their illness which can have a dramatic effect on their blood pressure whilst we also aim for early mobilisation to enhance the patients recovery when possible. Getting a patient’s blood pressure right really helps reduce their length of stay so it’s important.
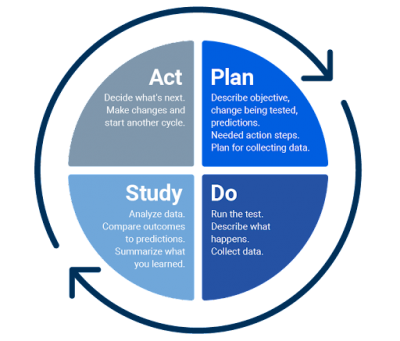
‘Vicki helped us approach the challenge with small tests of change, using Plan, Do, Study, Act (PDSA) cycles,’ Sarah explains. ‘These cycles allowed us to implement gradual improvements and evaluate their impact before wider implementation. We didn’t get it right first time and Vicki supported me to keep going. Stuck at 17% following the first two cycles, I decided to offer more education to the nursing team which demonstrated an improvement to 43% and subsequent involvement of our Lead Consultant saw results improve to 50%. Finally, we added a simple sticker to each patient’s documentation. The sticker raised awareness that everyone needed to have a test conducted and when this was not clinically possible served as a visual reminder to review this within 72 hours. It supports good communication within the team to ensure that the lying and standing BP test is completed in a timely way to best inform the patients care and treatment.’
As the team progressed through the PDSA cycles, compliance with blood pressure monitoring steadily increased—from 17% to 75%. ‘It’s not just about me leading the change,’ Sarah notes, ‘but about the whole team taking ownership. The culture shift has been remarkable. It’s brought us closer as a team and given everyone a voice in the process.’
The support from the Ward Accreditation team has also transformed Sarah’s leadership approach. ‘Before, I felt overwhelmed trying to manage too many things at once, running myself ragged, trying to do too many things at once. Now, I focus on leading the team, instigating change, and ensuring everyone is involved in monitoring and improving care, it’s given me confidence. This process has been an incredible experience for me personally and professionally.’
‘I now know that it’s ok to fail. Initially, I didn't want to see the results for the first PDSA. I wanted to get it right straight away and I saw failure as a weakness. But it was a learning process. And it was changing little bits each time and not changing the world. You need to change a little bit each time.’
‘For Sarah and the C4 team, this journey is not just about achieving accreditation—it’s about valuing each team member's contributions, promoting collaboration, and creating a positive ward culture that supports continuous learning and improvement. Sarah has demonstrated fantastic leadership and has been empowered to use her digital data to demonstrate how well the team are doing.’ Helen Bonello, Senior Nurse Professional Standards, Ward Accreditation and Improvement Programme.
Vicki adds, ‘Sarah’s commitment to improving patient safety demonstrates how small, focused changes can have a direct impact on patient care. This is a testament to the power of teamwork, continuous development, and a strong culture of shared responsibility.’
Lying and Standing Blood Pressure compliance on C4 Stroke. Collected via Tendable